每日外闻80
How does coronavirus kill? -7
冲击大脑1
COVID-19患者的另一组显著的症状集中在大脑和中枢神经系统。弗龙特拉说,她所在的医院需要神经科医生来评估5%到10%的冠状病毒患者。但她说,这“可能严重低估了”那些大脑处于斗争状态的人数,尤其是因为许多人使用了镇静剂和呼吸机。
弗龙特拉曾见过患有脑炎性脑炎,癫痫发作和“交感神经风暴”的患者,这是一种交感神经系统反应过度,可引起癫痫样症状,在脑外伤后最常见。一些COVID-19的患者会短暂地失去意识。其他会短暂失去意识的人一般患有中风。许多COVID-19的患者说他们失去了嗅觉。弗龙特拉和其他人想知道,在某些情况下,感染是否会抑制感觉氧气缺乏的脑干反射。这是对轶事性观察的另一种解释,即一些患者尽管血氧水平低到有生命危险的程度,但并没有气喘吁吁地呼吸空气。
约翰斯·霍普金斯医学院的重症监护医师罗伯特·史蒂文斯(Robert Stevens)说,ACE2受体存在于神经皮层和脑干中。但目前还不清楚病毒是在什么情况下穿透大脑并与这些受体相互作用的。也就是说,2003年非典(SARS)流行背后的冠状病毒—今天的罪魁祸首-COVID-19的近亲—可能会渗入神经元,有时还会引起脑炎。4月3日,《国际传染病杂志》(International Journal of Infectious Diseases)上刊登了一个来自日本的研究小组的案例研究报告。报告显示,在一名罹患脑膜炎和脑炎的covid19患者的脑脊液中发现了新冠状病毒的踪迹,这表明该病毒也可以穿透中枢神经系统。

*一名患有COVID-19的58岁女性患了脑炎,导致大脑组织受损(箭头)*N. POYIADJI ET AL., RADIOLOGY, (2020) DOI.ORG/10.1148/RADIOL.2020201187
Buffeting the brain 1
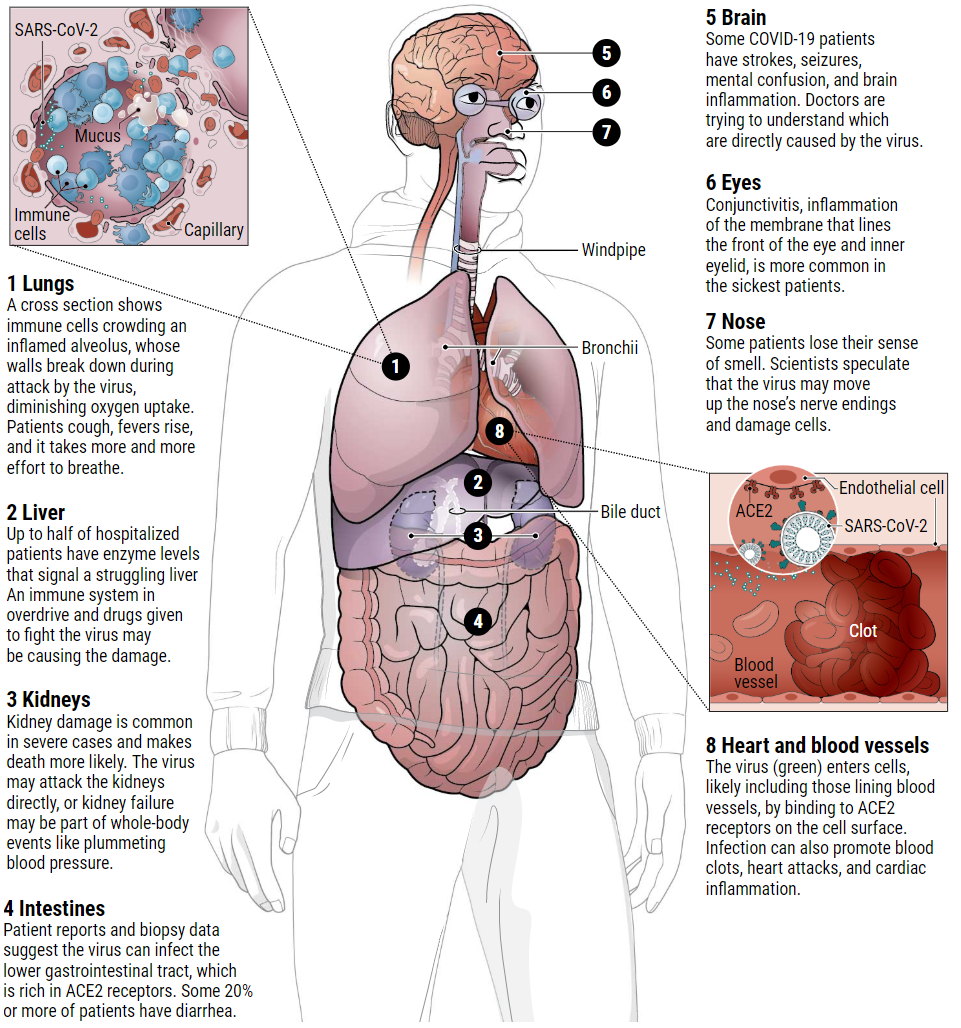
Another striking set of symptoms in COVID-19 patients centers on the brain and central nervous system. Frontera says neurologists are needed to assess 5% to 10% of coronavirus patients at her hospital. But she says that “is probably a gross underestimate” of the number whose brains are struggling, especially because many are sedated and on ventilators.
Frontera has seen patients with the brain inflammation encephalitis, with seizures, and with a “sympathetic storm,” a hyperreaction of the sympathetic nervous system that causes seizurelike symptoms and is most common after a traumatic brain injury. Some people with COVID-19 briefly lose consciousness. Others have strokes. Many report losing their sense of smell. And Frontera and others wonder whether in some cases, infection depresses the brain stem reflex that senses oxygen starvation. This is another explanation for anecdotal observations that some patients aren’t gasping for air, despite dangerously low blood oxygen levels.
ACE2 receptors are present in the neural cortex and brain stem, says Robert Stevens, an intensive care physician at Johns Hopkins Medicine. But it’s not known under what circumstances the virus penetrates the brain and interacts with these receptors. That said, the coronavirus behind the 2003 severe acute respiratory syndrome (SARS) epidemic—a close cousin of today’s culprit—could infiltrate neurons and sometimes caused encephalitis. On 3 April, a case study in the International Journal of Infectious Diseases, from a team in Japan, reported traces of new coronavirus in the cerebrospinal fluid of a COVID-19 patient who developed meningitis and encephalitis, suggesting it, too, can penetrate the central nervous system.

A 58-year-old woman with COVID-19 developed encephalitis, resulting in tissue damage in the brain (arrows).N. POYIADJI ET AL., RADIOLOGY, (2020) DOI.ORG/10.1148/RADIOL.2020201187
See you tomorrow