每日外闻79
How does coronavirus kill? -6
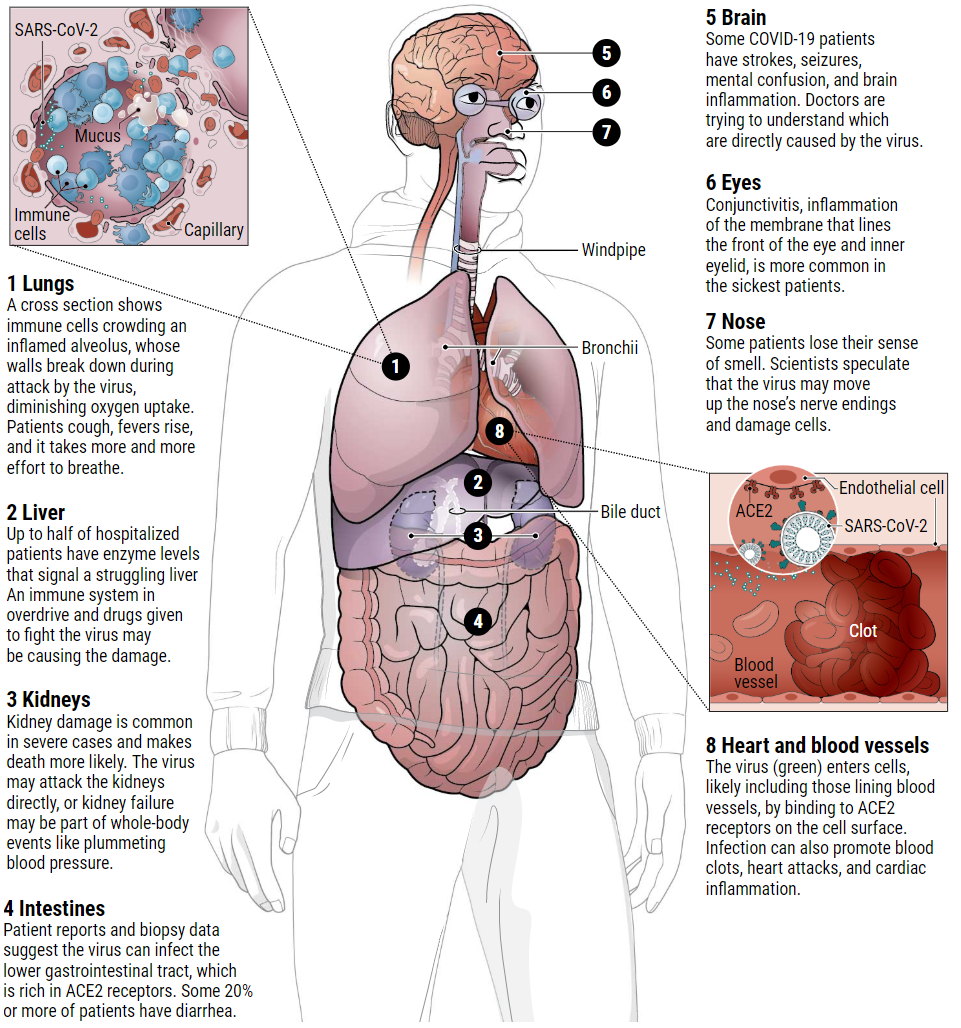
攻击身体的多个部位
全球范围内对呼吸机短缺(肺功能衰竭患者使用)的担忧引起了广泛关注。而对另一种设备——透析机的争抢就不那么激烈了。纽约大学朗格尼医学中心的神经学家弗龙特拉(Jennifer Frontera)说,如果这些人不是死于肺衰竭,那么他们就是死于肾功能衰竭。该中心治疗了数千名covid19患者。她所在的医院正在开发一种使用不同设备的透析方案,以支持更多的患者。需要透析的原因可能是因为肾脏富含ACE2受体,是另一个病毒的作用靶点。
据一项文章报道显示,武汉85名住院患者中有27%患有肾衰竭。另一份报告称,在中国湖北和四川两省近200名住院的covid19患者中,59%的患者尿液中含有蛋白质,44%的患者有血液;这两种情况都表明肾脏受损。那些患有急性肾损伤(AKI)的COVID-19患者,其死亡率是没有急性肾损伤的COVID-19患者的5倍多。

意大利的医护人员正在重症监护病房照顾一名19岁的covid19患者。
中国科学院苏州生物医学工程技术研究所神经科学家、该研究报道的共同作者贾洪波说:“肺是病毒主要的战场。但是一小部分病毒可能会攻击肾脏。就像在真实的战场上一样,如果两个地方同时受到攻击,每个地方都会变得更糟。”
有一项研究显示,在尸检的肾脏电子显微照片中发现了病毒颗粒,这表明肾脏被病毒直接的攻击过。但肾脏损伤也可能是附带损害。呼吸机增加了肾脏损伤的风险,抗病毒化合物包括瑞昔韦也会增加肾脏损害的风险,后者正在试验用于COVID-19患者。细胞因子风暴还能显著减少流向肾脏的血液,造成通常是致命的损害。而像糖尿病这样已经存在的疾病会增加肾脏受伤的几率。西北肾脏中心的首席医疗官Suzanne Watnick说,有很多已经患有慢性肾脏疾病的人有更高的急性肾脏损伤的风险。
Multiple battlefields
The worldwide fears of ventilator shortages for failing lungs have received plenty of attention. Not so a scramble for another type of equipment: dialysis machines. “If these folks are not dying of lung failure, they’re dying of renal failure,” says neurologist Jennifer Frontera of New York University’s Langone Medical Center, which has treated thousands of COVID-19 patients. Her hospital is developing a dialysis protocol with different machines to support additional patients. The need for dialysis may be because the kidneys, abundantly endowed with ACE2 receptors, present another viral target.
According to one preprint, 27% of 85 hospitalized patients in Wuhan had kidney failure. Another reported that 59% of nearly 200 hospitalized COVID-19 patients in China’s Hubei and Sichuan provinces had protein in their urine, and 44% had blood; both suggest kidney damage. Those with acute kidney injury (AKI), were more than five times as likely to die as COVID-19 patients without it, the same Chinese preprint reported.

Medical staff work to help a COVID-19 patient in an intensive care unit in Italy. ANTONIO MASIELLO/GETTY IMAGES
“The lung is the primary battle zone. But a fraction of the virus possibly attacks the kidney. And as on the real battlefield, if two places are being attacked at the same time, each place gets worse,” says Hongbo Jia, a neuroscientist at the Chinese Academy of Sciences’s Suzhou Institute of Biomedical Engineering and Technology and a co-author of that study.
Viral particles were identified in electron micrographs of kidneys from autopsies in one study, suggesting a direct viral attack. But kidney injury may also be collateral damage. Ventilators boost the risk of kidney damage, as do antiviral compounds including remdesivir, which is being deployed experimentally in COVID-19 patients. Cytokine storms also can dramatically reduce blood flow to the kidney, causing often-fatal damage. And pre-existing diseases like diabetes can increase the chances of kidney injury. “There is a whole bucket of people who already have some chronic kidney disease who are at higher risk for acute kidney injury,” says Suzanne Watnick, chief medical officer at Northwest Kidney Centers.
See you tomorrow