每日外闻75
How does coronavirus kill? Clinicians trace a ferocious rampage through the body, from brain to toes
How does coronavirus kill? -2
感染的开始
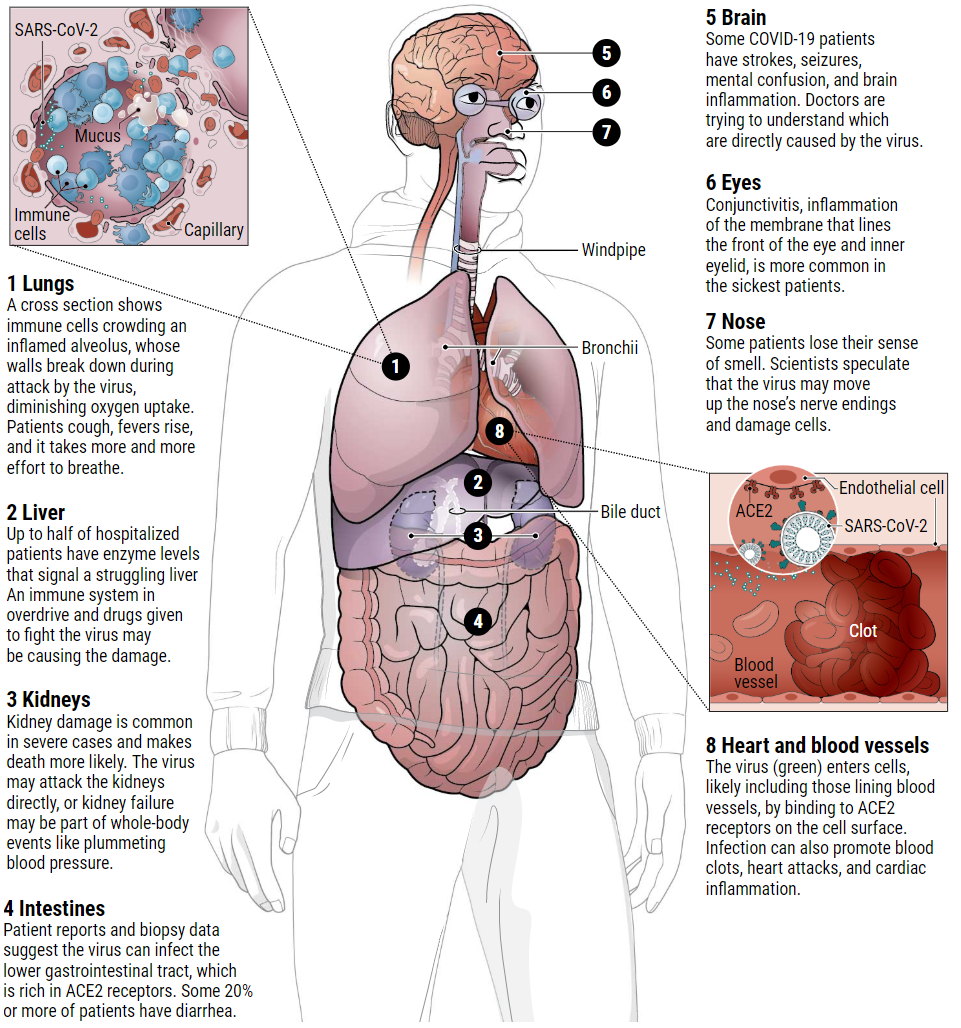
当被感染者咳出携带病毒的飞沫,被其他人吸入后,新型冠状病毒(SARS-CoV-2)就会进入鼻腔和咽喉。根据韦康桑格研究所(Wellcome Sanger Institute)和其他机构的科学家的研究资料表明,它在鼻子内壁找到了一个受欢迎的归宿。他们发现那里的细胞富含一种叫做血管紧张素转换酶2 (ACE2)的细胞表面受体。在人体各处,ACE2的存在标志着组织易受感染,因为病毒需要这种受体进入细胞。ACE2通常情况下有助于调节血压。病毒一旦进入细胞内部,就会劫持细胞的这个“工厂”,复制无数个自己,并侵入新的细胞。
随着病毒的繁殖,感染者可能会排出大量的病毒,特别是在第一周左右。此时可能还没有临床上的感染症状。或者,病毒的新宿主可能会出现发烧、干咳、喉咙痛、嗅觉和味觉丧失,或者头痛和身体疼痛。
如果免疫系统在病毒感染的最初阶段没有击退它(SARS-CoV-2),那么病毒就会沿着气管向下蔓延,攻击肺部,进而导致死亡。肺呼吸树的较细、较远的分支一直延伸到称为肺泡的微小气囊中,每个气囊由单层细胞排列,这些细胞也富含ACE2受体。
正常情况下,氧气通过肺泡进入毛细血管-位于肺泡旁的微小血管,然后氧气被输送到身体的其他部位。但是当免疫系统与入侵者作战时,战斗本身就会破坏这种正常的氧气传输。战斗前线的白细胞释放一种叫做趋化因子的炎症分子,这些趋化因子反过来又会召唤更多的免疫细胞来瞄准并杀死被病毒感染的细胞,留下大量的液体和死细胞-也就是脓汁。这是肺炎的基本病理过程,其伴有有相应的症状:咳嗽、发烧、呼吸又快又浅。一些covid19患者可以康复,但有时只能依靠呼吸机的鼻套管吸入氧气。
但是其他的病情恶化,像一种叫做急性呼吸窘迫综合症(ARDS)的疾病发病通常是很突然的。这种疾病的患者血液中的氧气含量急剧下降,相比于普通肺炎患者,呼吸变得更加困难。在x光和计算机断层扫描中,他们的肺部满是白色的混浊物,而在正常的肺中,这些混浊物的位置本该是黑色-表示这个部位有空气。一般情况下,这些病人最终需要使用呼吸机来帮助呼吸。他们中有很大一部分的人都死了。尸检结果显示,他们的肺泡中充满了液体、白细胞、粘液和被破坏的肺细胞的碎屑(见图)。

The infection begins
When an infected person expels virus-laden droplets and someone else inhales them, the novel coronavirus, called SARS-CoV-2, enters the nose and throat. It finds a welcome home in the lining of the nose, according to a preprint from scientists at the Wellcome Sanger Institute and elsewhere. They found that cells there are rich in a cell-surface receptor called angiotensin-converting enzyme 2 (ACE2). Throughout the body, the presence of ACE2, which normally helps regulate blood pressure, marks tissues vulnerable to infection, because the virus requires that receptor to enter a cell. Once inside, the virus hijacks the cell’s machinery, making myriad copies of itself and invading new cells.
As the virus multiplies, an infected person may shed copious amounts of it, especially during the first week or so. Symptoms may be absent at this point. Or the virus’ new victim may develop a fever, dry cough, sore throat, loss of smell and taste, or head and body aches.
If the immune system doesn’t beat back SARS-CoV-2 during this initial phase, the virus then marches down the windpipe to attack the lungs, where it can turn deadly. The thinner, distant branches of the lung’s respiratory tree end in tiny air sacs called alveoli, each lined by a single layer of cells that are also rich in ACE2 receptors.
Normally, oxygen crosses the alveoli into the capillaries, tiny blood vessels that lie beside the air sacs; the oxygen is then carried to the rest of the body. But as the immune system wars with the invader, the battle itself disrupts this healthy oxygen transfer. Front-line white blood cells release inflammatory molecules called chemokines, which in turn summon more immune cells that target and kill virus-infected cells, leaving a stew of fluid and dead cells—pus—behind. This is the underlying pathology of pneumonia, with its corresponding symptoms: coughing; fever; and rapid, shallow respiration. Some COVID-19 patients recover, sometimes with no more support than oxygen breathed in through nasal prongs.
But others deteriorate, often quite suddenly, developing a condition called acute respiratory distress syndrome (ARDS). Oxygen levels in their blood plummet and they struggle ever harder to breathe. On x-rays and computerized tomography scans, their lungs are riddled with white opacities where black space—air—should be. Commonly, these patients end up on ventilators. Many die. Autopsies show their alveoli became stuffed with fluid, white blood cells, mucus, and the detritus of destroyed lung cells (see graphic).
See you tomorrow